As the 4 July UK general election looms on the horizon, experts say that the UK clinical trial landscape could be due for a significant makeover.
Ahead of a nationwide election, major UK political parties have promised ways to revamp the healthcare system. The Labour party has proposed measures to establish a maximum of 18 weeks from referral to consultant-led treatment of non-urgent health conditions amongst other actions. On the other hand, the Conservative party has pledged to increase National Health Service (NHS) spending above inflation each year. However, alongside the broader healthcare policies, the UK’s pharmaceutical and clinical trials industry also stands to experience change.
Last year, the former health minister, Lord James O’Shaughnessy led a review of the UK commercial clinical trial landscape that outlined major areas for improvement. After the review, the government set forth aims to tackle O’Shaughnessy’s recommendations already making some major progress towards some of the review’s goals.
In such a backdrop, experts at the Annual Outsourcing in Clinical Trials UK and Ireland conference in London, held earlier this month, debated ways to improve the UK’s standing in the global clinical research market, amidst conversations about artificial intelligence (AI), clinical trials in the APAC region, and more.
UK Clinical landscape
At the conference, Dr. Andrew Ustianowski, the network director at the National Institute for Health and Care Research’s (NIHR) North West Regional Research Delivery Network, highlighted the Vaccine Innovation Pathway’s March 2024 launch of a funding call, and clearance of the MHRA backlog as significant steps forward. He reported that, as of May 2024, 79% of open UK clinical studies were “delivering to time and target”. However, he called attention to new important areas of improvement.
Ustianowski said that the UK needs to boost the speed of its timelines for clinical trial approval to catch up to international standards. O’Shaughnessy highlighted that statistics show that UK clinical trials are carried out twice as slow as the US trials, and a third slower than those in Australia and Spain. Moreover, sponsors make their regulatory submissions to the UK later than other countries, added Ustianowski. O’Shaughnessy offered the potential solution of evaluating the functionality of the current framework against those of other countries. He said that the UK commonly approaches appraisals of its system through comparison to previous versions.
APAC’s potential as a clinical hub
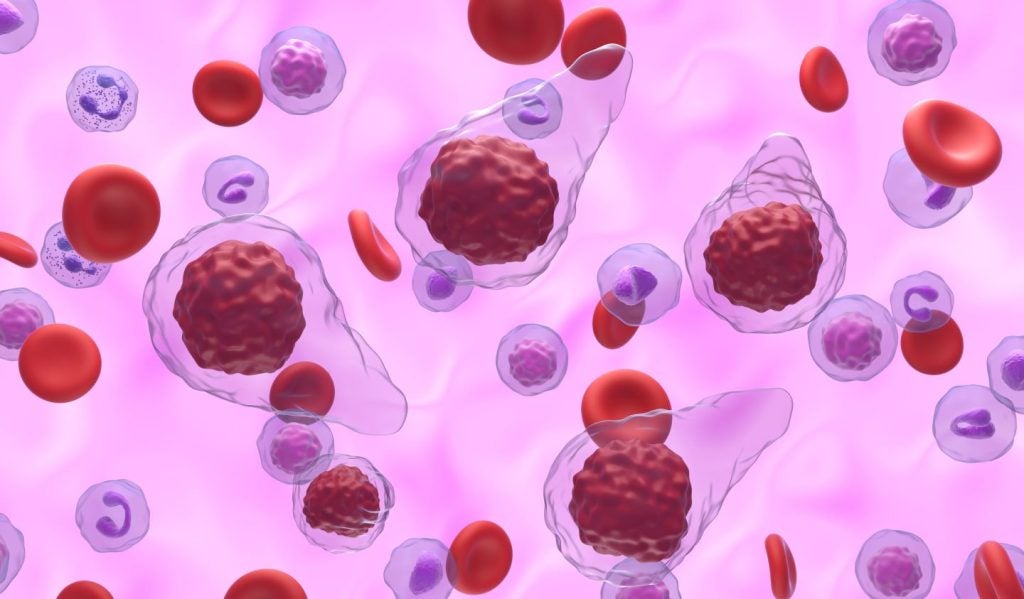
The conference also highlighted rising trends in the clinical trial landscape towards therapeutic development in the Asia-Pacific (APAC) region. A presentation from Scotty Chung-Siu, a GlobalData managing analyst, reported that the APAC region is leading the clinical development of adoptive cell therapies. GlobalData reports that there are 1,072 ongoing adoptive cell therapy trials in the APAC region, compared to 569 in the US, as of 20 June.
GlobalData is the parent company of Pharmaceutical Technology.
At a session on clinical research in the APAC region, Dr. Yooni Kim, the vice president of clinical services at Novotech, explained the pros of research in APAC geographies, while focusing on specific countries. For example, Kim highlighted that in Taiwan, regulators freely accept trial protocols that match standards from German, Japanese and French systems, amongst other countries. She said that this could help companies shorten timelines for clinical studies.
Kim also directed attention to South Korea, where the government has developed a national AI platform that integrates data from various healthcare institutions to support clinical trials. At a talk on AI in clinical research, Josep Bori, the research director of GlobalData’s Thematics division, highlighted AI’s potential to manage and engage with patients and manage healthcare data, amongst other things. Kim said South Korea’s platform is already helping companies with these tasks by monitoring clinical trials and recruiting patients for studies more efficiently. O’Shaughnessy’s 2023 review highlighted a similar need for more data integration in the UK system, which was discussed on the second day of the conference.
Data integration
At the last keynote session of the event, O’Shaughnessy called attention to the need “to take advantage of the NHS’s considerable data assets”. At the same time, he highlighted that there is a lack of transparency around data collected during commercial clinical activity in the UK. In one of the related sessions, a clinical research professional in the audience, pointed out that while most research institutions and companies have independent data collection measures, they are unable to share it properly without a universal platform for the industry. Nonetheless, the former health minister shared hopes that the next government would prioritise the provision of “real-time data” on the UK’s commercial clinical activity.