On 16 June, 2024, during the European Hematology Association (EHA) 2024 Hybrid Congress in Madrid, Spain, new positive results from the randomised, double-blind, placebo-controlled Phase III ECHO clinical trial were presented on AstraZeneca’s Calquence (acalabrutinib).
The trial tested the drug in combination with chemoimmunotherapy, bendamustine and Roche/Biogen’s MabThera (rituximab) as first-line therapy for mantle cell lymphoma (MCL). The trial results suggest that this Calquence combination therapy could become a new standard-of-care (SOC) for older patients (>65 years) with MCL, who are ineligible for autologous stem cell therapy, as it shows potential to extend survival for the first time.
MCL is a rare and often severe form of non-Hodgkin lymphoma (NHL) that develops when B lymphocytes transform into malignant cells in the mantle zone of a lymph node and is frequently diagnosed in the late stages. MCL accounts for about 5% of NHL cases. According to GlobalData’s epidemiology data, MCL has an annual incidence rate of one per 100,000 population across the seven major markets (the US, France, Germany, Italy, Spain, the UK, and Japan). Calquence is a next-generation selective irreversible Bruton's tyrosine kinase (BTK) inhibitor. It covalently binds a cysteine residue (Cys481) in the BTK active site and inhibits BTK enzymatic activity, suppressing malignant B-cell proliferation and survival.
In the ECHO trial, 598 patients (299 per arm) with a median age of 71 years, were evenly distributed between the experimental (acalabrutinib + bendamustine + rituximab; ABR) and control (placebo + bendamustine + rituximab; PBR) treatment arms. After a median follow-up of 45 months, the ABR arm had a higher overall response rate (91.0% vs. 88.0%) and complete response rate (66.6% vs. 53.5%) than the PBR arm. The median progression-free survival (PFS) was prolonged in the ABR arm (66.4 months vs. 49.6 months, HR 0.73, P=0.0160). The secondary endpoint, overall survival (OS), favoured ABR. However, it was not statistically significant (HR 0.86, P=0.27), and the trial will continue to evaluate OS.
Covid-19 deaths influenced trial results, with both arms showing increased median PFS following censoring for Covid-19 deaths. In the ABR arm, the censoring reduced the risk of disease progression or death by 36%. The safety profiles were comparable, with an identical incidence of grade ≥3 adverse events (AEs) (88.9% for ABR and 88.2% for PBR). Covid-19-related events and pneumonia were more common in the ABR group, resulting in a higher discontinuation rate for AEs (42.8% vs. 31.0%). During the presentation, the investigator mentioned that 80% of patients in both trial arms received the Covid-19 vaccination.
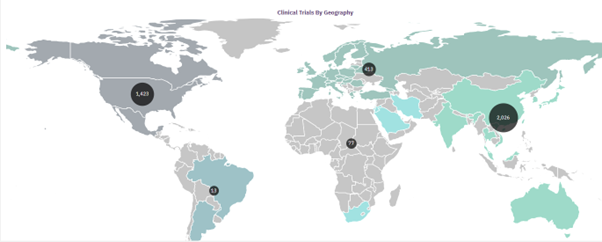
According to GlobalData's analyst consensus forecast, Calquence will generate global sales of over $4bn by 2030. Currently, several BTK inhibitors are in Phase III clinical trials as front-line therapy for MCL patients, including BeiGene’s Brukinsa (zanubrutinib), Eli Lilly's Jaypirca (pirtobrutinib), InnoCare’s Inokai (orelabrutinib), and AbbVie/J&J’s Imbruvica (ibrutinib). If Calquence receives FDA label expansion in MCL, it will achieve a unique position in the treatment-naive MCL market share.
However, this will depend on how quickly AstraZeneca can file for FDA approval, as AbbVie/J&J had to withdraw the accelerated FDA approval because a Phase III confirmatory trial (SHINE) revealed no OS advantage and a 7% increase in the risk of death in the Imbruvica arm. Another next-generation BTK inhibitor competitor to watch for, as first-to-market Imbruvica has lost favor, is Brukinsa, which can get ahead in the race if it shows superior efficacy and safety profiles compared to Calquence plus chemoimmunotherapy.