The European Commission (EC) has awarded conditional marketing authorisation for Pfizer's DURVEQTIX (fidanacogene elaparvovec), a one-time gene therapy for use in adults with severe and moderately severe haemophilia B.
The medicine is indicated for use in patients without a history of factor IX inhibitors and detectable antibodies to variant AAV serotype Rh74.
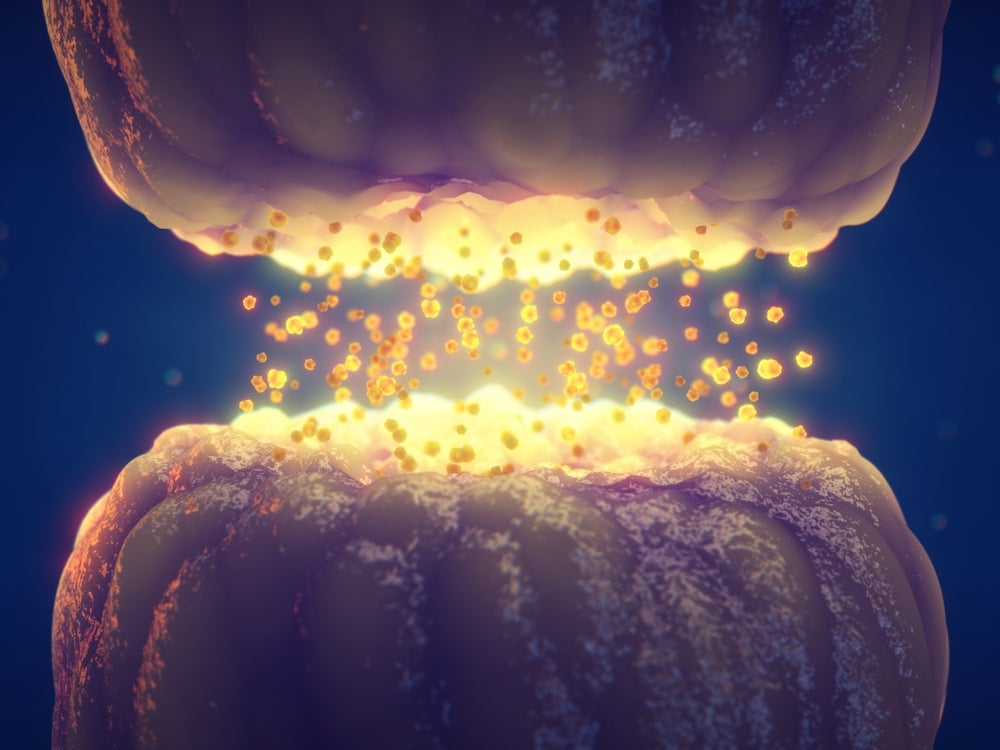
DURVEQTIX enables haemophilia B patients to produce factor IX themselves, eliminating the need for multiple weekly or biweekly intravenous infusions.
The approval is based on the Phase III BENEGENE-2 clinical trial data, which assessed the efficacy and safety of DURVEQTIX in adult male participants aged 18 to 62 years with haemophilia B.
The study met its primary efficacy endpoint, showing a statistically significant decline in annualised bleeding rate for total bleeds post-treatment compared to the prophylaxis regimen.
Efficacy remained stable from the second to the fourth year after treatment, and DURVEQTIX was generally well-tolerated, with a safety profile consistent with Phase I/II data.
This conditional marketing authorisation is valid across the 27 EU member states and in Liechtenstein, Iceland and Norway.
The therapy has also been approved by the US Food and Drug Administration and Health Canada, where it is marketed as BEQVEZ.
The company reported positive data from a Phase III programme for gene therapy in haemophilia A (giroctocogene fitelparvovec).
A Phase III trial is underway for marstacimab, an investigational treatment for people with haemophilia A and B, with and without inhibitors.
Pfizer chief international commercial officer and executive vice-president Alexandre de Germay said: “There is a substantial medical and treatment burden for people with haemophilia B that receive standard of care today, with frequent infusions and many remaining at risk of breakthrough bleeds that can lead to pain and restricted mobility.
“DURVEQTIX has shown the potential to offer long-term bleed protection in a one-time dose, reducing or eliminating bleeds for the appropriate patients with haemophilia B. These outcomes and their impact could become potentially transformative for haemophilia B care in the European Union.”