
Two gene therapies up for approval this year for sickle cell disease could be cost effective in some cases at a $2 million price point, based on a draft evidence report published by the Institute for Clinical and Economic Review (ICER).
Released on April 12, the report focuses on bluebird bio’s lovotibeglogene autotemcel and Vertex Pharmaceuticals and CRISPR Therapeutics’ exagamglogene autotemcel or exa-cel and their potential use in treating sickle cell disease. Although the findings in the report are only preliminary, they shed light at the considerations behind the high price tags of gene therapies.
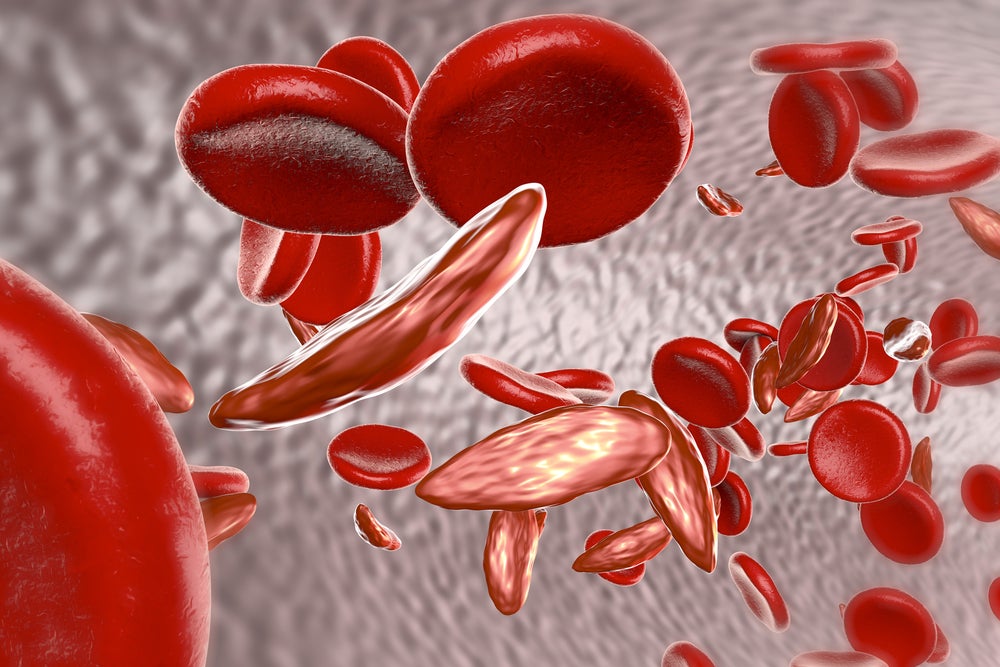
Sickle cell disease is an inherited blood disorder that is caused by mutations in the HBB gene, which codes for the oxygen-carrying protein haemoglobin in red blood cells. According to the Centers for Disease Control and Prevention (CDC), sickle cell disease affects roughly 100,000 Americans. The standard of care for the condition includes blood transfusions, hydroxyurea and iron chelation. While stem cell transplants can cure the condition, their use is limited due to some of the risks that come with them.
Also known as lovo-cel, bluebird bio’s product is a lentiviral gene therapy. Bluebird already uses a lentiviral vector in its approved gene therapy for beta-thalassemia called Zynteglo.
However, Vertex and CRISPR’s exa-cel is designed to remove a part of the patient’s BC11A gene to increase foetal haemoglobin levels in red blood cells, using CRISPR editing. While Vertex and CRISPR submitted the Biologics License Application (BLA) for exa-cel earlier this April, bluebird has yet to do so for lovo-cel. If approved, exa-cel would be the first FDA-approved gene therapy based on CRISPR editing.
Since the price of the therapies is unknown, the institute used a placeholder cost of $2 million. ICER uses quality-adjusted life year (QALY), a cost effectiveness metric to measure the value of a healthcare intervention. As per ICER, if a treatment improves quality of life or extends a patient’s life, then this can be represented in additional QALYs provided by the therapy. Based on the report’s QALY-based threshold analyses, both treatments would have to have a unit price of $1.58 million to achieve $150,000 per QALY gained from a healthcare system perspective. The treatments would have to cost $1.92 million to achieve a $200,000 QALY gained from the same perspective.
According to the report’s probabilistic sensitivity analysis, both therapies had a 0% probability of cost effectiveness at the threshold of $150,000 per QALY (and lower) from a healthcare system perspective. At the $200,000 threshold, “lovo-cel had a 27% probability of being cost effective and exa-cel had a 21% probability” from the same perspective.
Ultimately, the report states that both therapies resulted in “lifetime health gains and added costs when compared to standard of care alone”. The report adds that both therapies have an “incremental cost effectiveness that is above commonly cited thresholds from the health care system perspective”.
The use of lovo-cel compared to the standard of care for severe CDC is incremental or better, while the use of exa-cel versus standard of care is comparable or better, per the report. Still, comparing the two therapies remains difficult, with ICER rating the evidence as insufficient.
The report states that both therapies are “likely to substantially improve quality and length of life.” At the same time, the publication states that the cost effectiveness will depend on the eventual cost of the treatments.
Cell & Gene Therapy coverage on Pharmaceutical Technology is supported by Cytiva.
Editorial content is independently produced and follows the highest standards of journalistic integrity. Topic sponsors are not involved in the creation of editorial content.