Only a few weeks into the new year, the prospect of getting a successful advanced HIV vaccine shrank after the discontinuation of yet another late-stage trial.
On January 18, Janssen, a Johnson & Johnson (J&J) subsidiary, stated that its vaccine was not effective in preventing HIV infections. This marks the second time one of Janssen’s HIV vaccines failed after another showed disappointing results in the Phase IIb Imbokodo trial in August 2021.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
The failure of several late-stage trials highlights the challenging nature of HIV vaccine development. Since HIV integrates with the DNA, eliminating the virus from the body is very difficult, explains David Montefiori, PhD, director of the Laboratory for AIDS Vaccine Research and Development at Duke University in Durham, North Carolina. Once a patient is infected with HIV, they are infected for life, except for a few rare cases, he says.
While vaccines like those against Covid-19 are designed to prevent serious illness and death, HIV vaccines are meant to prevent infection. “Right away, that sets the bar high, because that means that we need a vaccine that will prevent the acquisition of infection altogether,” says Montefiori.
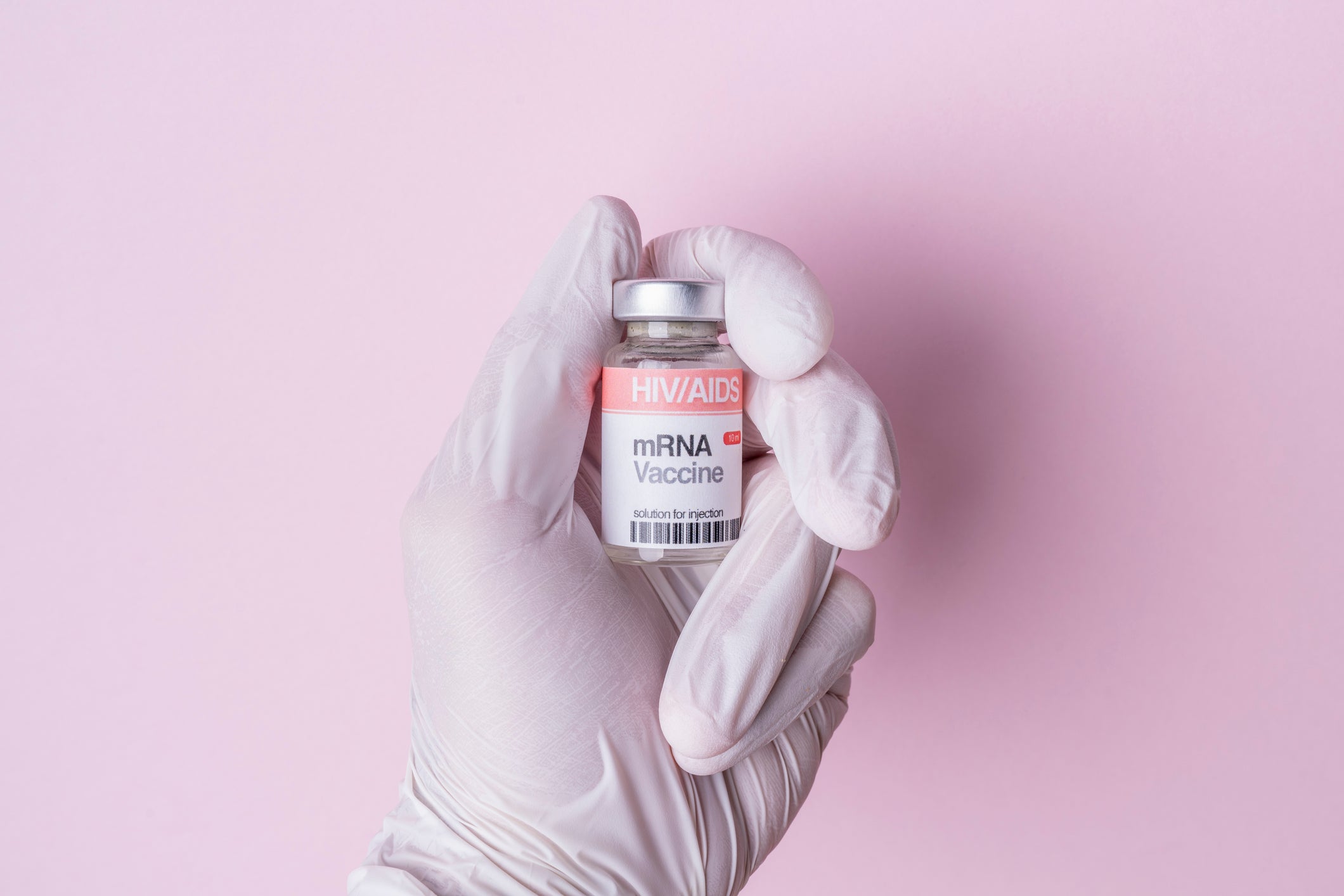
Now, the HIV research community is setting its sights on vaccines that are in earlier stages of development, based on new approaches like messenger RNA (mRNA)-based vaccines or those using human cytomegalovirus (HCMV) vectors. Additionally, advances in the study of broadly neutralising antibodies (bNAbs) have led to new candidates being studied in early trials.
A partial change in perspectives
The RV144 trial that took place between 2003 and 2006 in Thailand reported modest efficacy results, which generated enthusiasm for vaccines that induce responses from non-neutralising antibodies, says Montefiori. The study was done in collaboration with the United States Army Medical Research and Development Command (USAMRDC), the Thai Ministry of Health, and others. The trial tested a regimen featuring Sanofi’s recombinant canarypox vector vaccine ALVAC-HIV and two booster injections of the recombinant glycoprotein 120 subunit vaccine AIDSVAX produced by VaxGen.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataStarting in 2016, the South African Uhambo HVTN 702 study, studied the ALVAC vaccine followed by a different booster, but the trial was unsuccessful.
The Janssen vaccines studied in the Imbokodo and Mosaico studies were based on the mosaic concept, where they were intentionally designed to include a broader immunogen that could be used everywhere, says Dr. Mary Marovich, director of the Vaccine Research Program at National Institute of Allergy and Infectious Diseases (NIAID). Both studies featured a vaccine that was delivered using the adenovirus serotype 26 vector (Ad26), which was also a part of the J&J Covid-19 vaccine. Mosaico was a collaboration between the NIAID, Janssen, USAMRDC, and others. Imbokodo was also sponsored by the Bill & Melinda Gates Foundation.
Mosaico’s failure is a reminder of how complex HIV is as a virus, says Dr. Kundai Chinyenze, director of the International AIDS Vaccine Initiative’s (IAVI) Africa team. While the trials did not report significant efficacy, they still indicated signals that mandated further study, in the view of some researchers. In Imbokodo, two parts of the immune response seemed to correlate with protection, one of which is the activity of antibodies to the V1 and V2 regions of the envelope protein, says Susan Zolla-Pazner, PhD, professor of medicine at the Icahn School of Medicine at Mount Sinai, New York City. This response was also seen in the RV 144 trial, she notes. But others in the research space are now testing out other concepts that have been largely theoretical.
A move toward bNAbs
There are several promising approaches being studied in the early stages of development, and those focusing on generating bNAbs are particularly interesting, says Chinyenze.
While prior vaccines largely focused on T cell development to kill infected cells, these do not necessarily work well at preventing initial transmission, says Dr. Steven Deeks, professor of medicine at the University of California, San Francisco. To truly prevent transmission from the first day the virus appears in the tissue, there needs to be something that can block any cell from being infected, and bNAbs could achieve this, says Deeks. Even though the immune system makes antibodies in response to a virus, HIV mutates too quickly, and the created antibodies cannot target the virus, explains Dr. Salim Abdool Karim, director of the Centre for the AIDS Program of Research in South Africa (CAPRISA). However, in rare cases, some individuals can make bNAbs that target multiple strains of HIV, he explains.
While the production of bNAbs is a complicated process, vaccines could be designed to prompt the body to induce bNAbs, says Karim. The IAVI is studying vaccines that use a bNAb-focused approach in several trials. The first among these, IAVI G001, had positive Phase I results published in Science in December 2022. Conducted in collaboration with Scripps Research and other institutions, the study investigated the effect of the eOD-GT8 60mer immunogen, and found that it induced a targeted response in 97% of vaccinated subjects.
Additionally, the Phase I results added weight to germline targeting, a concept where bNAb precursor B cells are stimulated to eventually develop bNAbs, says Marovich. This could mean that multiple jabs are needed for the vaccine to successfully work, says Deeks. “We believe we’re going to need multiple different vaccines that will gently coax the immune system to make these bNAbs,” he says. The question now is how to design additional immunogens to create bNAbs from these precursor cells, says Montefiori. At the same time, this approach can be challenging, as it requires further additional vaccinations for necessary maturation, says Peter Kwong, PhD, chief of the Structural Biology Section at the NIAID.
IAVI now aims to complete the IAVI G002 and IAVI G003 trials, which are testing the delivery of these immunogens through an mRNA platform by July, confirms Chinyenze. The trials will test distinct immunogens in different population and are being done in collaboration with Scripps Research, the Bill & Melinda Gates Foundation, and other partners.
These newer vaccine approaches aim to induce different kinds of antibodies, and the mRNA delivery platform offers the advantage of faster vaccine manufacturing and increases the field’s capacity to study different immunogens or vaccine strategies simultaneously, says Chinyenze. mRNA vaccines can be made and modified quickly compared to protein subunit vaccines, says Montefiore.
Other ongoing HIV vaccine trials
While mRNA vaccines continue to stay in the limelight, other approaches are also being investigated for HIV. Vir Biotechnology is developing a HCMV-based vaccine, which is currently in a Phase I trial. While data from the first two cohorts did not show any HIV insert-specific T cell response, a third cohort readout is expected in H1 2023. Since this is a first-in-human study, the vaccine’s safety profile still needs to be understood, which explains why the first two cohorts received low doses, says Deeks. The third cohort features the highest studied dose.
At even earlier stages of development, Kwong aims to push an epitope-based vaccine approach into the clinic at the NIAID next year.
“The cutting edge of vaccinology has always been with HIV,” says Deeks. “Even though we do not necessarily make great progress with HIV, we make great progress for everything else. It is hard to predict the future, [but] right now, people are on the cutting edge of science.”


