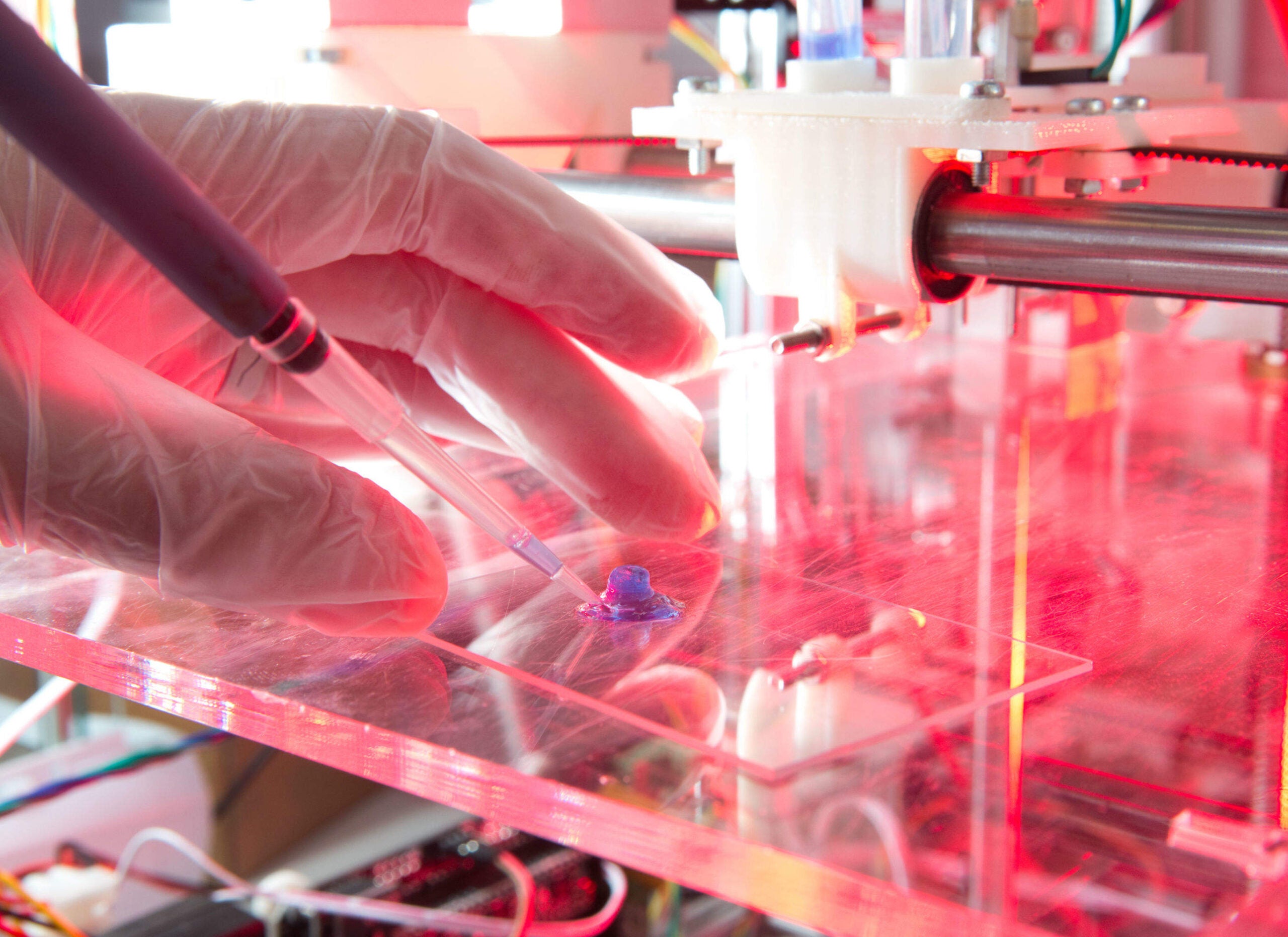

In October 2015, researchers at Heriot-Watt University hit the headlines with a remarkable new 3D printing process. Their technique, the first of its kind in the world, allows them to print human stem cells derived from a donor’s own tissues. The possibilities are radical – it could pave the way for lab-grown human tissues for use in pharmaceutical research, and ultimately replacement organs.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
This wasn’t the first time the team had announced such a breakthrough. Nearly three years ago, the researchers – who belong to Heriot-Watt’s Biomedical Microengineering Group in collaboration with Roslin Cellab – created the first 3D printer capable of printing embryonic stem cell cultures. Prior to this point, human stem cells were considered too sensitive to manipulate in this way, and the development was said to have "immensely valuable long-term implications".
To date, however, the applications of embryonic stem cells have been disappointingly limited. Beset by regulatory clampdowns across the world, not to mention technical challenges, their potential remains mostly unrealised. As Dr Will Shu explains, printing human embryonic stem cells was never his team’s end game.
"Although they are very useful, they involve some ethical issues – you have to destroy human embryos," says Shu, from the School of Engineering and Physical Sciences at Heriot-Watt. "Because of that, we focused on working toward the printing of an even more delicate cell source – human induced pluripotent stem (iPS) cells. These work like a human embryonic stem cell, but the source is an individual person rather than an embryo."
Tweaking the technique
This form of stem cell, first generated in 2006 by the Nobel Prize winning Shinya Yamanaka, comes about when an adult cell (for example from skin or muscle tissue) is reprogrammed back into a pluripotent stage through the introduction of a particular set of genes.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataLike embryonic stem cells, they can self-renew indefinitely, and can be differentiated into any adult cell type as necessary. Unlike embryonic stem cells, however, they are not ethically contentious. What is more, because they can be taken from the patient who is due to receive the transplanted tissues, they are suitable for autologous therapies and are unlikely to be rejected by the patient’s immune system.
Being able to 3D print these cells is, therefore, a major step forward – but it was far from being a simple task.
"The challenge is that human iPS cells are an even more delicate cell source and they’re very difficult to manipulate," says Shu. "We needed to significantly modify our printing technology to make it even more gentle towards the cells."
Like their previous cell printing platform, the new technique is valve-based, involving nanolitre dispensing systems for bio-ink solution. But it is also smaller and lighter, and the electronics are more robust, improving its reliability and speed. This enables the team to print the cells in three dimensions without adversely affecting their biological functions.
Reporting their work in the IOP journal Biofabrication, Shu and colleagues described how, after printing, the cells were cultured for several weeks. The team then used a specially designed protocol to differentiate the stem cells into liver cells, demonstrating that they remained viable and pluripotent.
"Because these cells can replicate outside the body forever, you can produce unlimited sources of these useful cell types," says Shu. "The bio-ink used in our 3D printing becomes the material for producing, for example, human liver tissue."
An end to animal testing?
In the short term, the team hopes to create human micro-tissues suitable for drug testing. Currently, drug development is a drawn-out process, taking around 9-12 years on average, with a high failure rate. This is partially due to the fact that many drugs are not tested on humans until a late stage of development. Although they have been tested as safe in animals, they are later shown to have toxic effects for human patients.
Through using miniature human tissues, derived from 3D printed stem cells, a drug’s toxicity in humans could be more readily ascertained. This would not only create a more reliable and scalable drug testing platform, but would hopefully put an end to the ethical issues surrounding animal testing.
"Using our technology, you can test the liver toxicity of any potential pharmaceutical drug candidates directly using human tissue rather than animals, so that’s our short-term objective," explains Shu.
There are direct implications here for personalised medicine, in that each micro-tissue functions as a direct model of the donor’s own cells. Once the technology is established, it should be possible to model a patient’s individual response to a drug, therefore enabling better targeted medicines. It may also improve understanding of particular diseases, allowing tissue engineers to use iPS cells sourced from donors with specific conditions to create new models of that disease.
Ending organ shortages
In the longer term, technologies of this kind have been touted as holding great promise for organ donation. The problems associated with organ shortages are well known; currently most potential recipients on waiting lists die before they can receive a donor organ, with transplant supply meeting less than 10% of the global demand. Even if a transplant is performed, there may be problems with rejection, and the recipient will probably have to take immunosuppressant drugs for the rest of their life.
If human organs, derived from the recipient’s own stem cells, could be bioengineered in a lab, these difficulties could be a thing of the past.
"Obviously we would like to 3D print organs using our technology, using different types of cells generated from these stem cell sources, so that we don’t have to rely on organ donation in the future," says Shu. "The organs generated by this process would not be rejected, because the cells are from an individual person, leading to personalised organ regeneration."
While that long-term goal is not on the radar for now, the Heriot-Watt team has undoubtedly taken an important step forward in regenerative medicine. As the researchers fine-tune their printing platform, and work with industry partners to apply their technology, it seems clear that the principle is more than ready to be put into practice.
"If there are any pharmaceutical companies who would like to test their drug using our platform, we’re always happy to talk to them," says Shu.




