
On 16 February 2016, the headlines were unambiguous: "T-cell therapy offers lasting cure prospects"; "New cancer therapy could give hope to ‘incurable’ patients"; "Cancer researchers claim ‘extraordinary’ results". While breakthroughs in oncology are hardly unusual – with incremental developments par for the course – this was surely the biggest and most exciting in some time.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
The treatment in question, chimeric antigen receptor (CAR) T-cell therapy, had been given to nearly 100 patients suffering from advanced blood cancers in three separate clinical trials. These patients had all failed other treatments, and the majority had between two and five months to live. However, with the experimental new therapy, the turnaround was remarkable: they not only extended their lifespans, but showed complete remission after 18 months.
In one trial, 29 patients with otherwise incurable, or constantly relapsing, acute lymphoblastic leukaemia underwent the immune cell therapy. All but two of them (93%) fully recovered. Similar results applied to participants with non-Hodgkin’s lymphoma and chronic lymphocytic leukaemia. In these trials, around 80% responded to treatment, with more than half experiencing complete alleviation of symptoms.
The treatment was not being pegged as a miracle cure: a number of patients had suffered debilitating side effects, and two had died. However, it stood to reason that the researchers, presenting at the American Association for the Advancement of Science (AAAS) annual meeting, were galvanised.
"This is unprecedented in medicine, to be honest, to get response rates in this range in these very advanced patients," said Professor Stanley Riddell, an immunotherapy researcher at the Fred Hutchinson Cancer Research Centre, whose team was responsible for the findings.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataWhile conceding that researchers had "a long way to go", he described the results as "potentially paradigm-shifting" – strong words from a profession allergic to hyperbole. Another researcher in the field, Professor Chiara Bonini of the University Vita-Salute and San Raffaele Scientific Institute in Milan, described the latest wave of findings as "really a revolution," adding: "I think we are at the beginning of a road."
An elegant technique
So is the buzz truly justified? Despite giving the appearance of an overnight success story, research in the field already began in the late 1980s, when an Israeli chemist developed the first CAR T-cells. Over the next two decades, the associated technologies developed steadily – stealthily even – as the teething problems were ironed out.
In recent years, with the technology reaching a critical juncture, T-cell therapy has seen a huge influx of funding. Since late 2013, a number of pharma companies have forged multimillion dollar deals and have planned dozens of clinical trials. With immunotherapy pegged as a key new research avenue, one 2014 Forbes headline brazenly asked of the treatment: "Is this how we’ll cure cancer?"
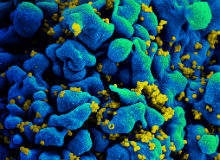
T-cell therapy involves extracting a patient’s T-cells from their blood and modifying them with a targeted antibody, in this case a chimeric antigen receptor that identifies cancer cells. The cells are then infused back into the bloodstream, where they quickly home in on tumour cells. This not only kills the cancer; it also prevents its recurrence.
While the technique sounds elegant, it is not without its pitfalls, and it has taken many years to reach a point where the therapy can be viably used in humans. One of the issues has been ensuring the consistency of the CAR T-cells, which, if unstable, can cause side effects such as cytokine release syndrome along with unpleasant neurological symptoms. Riddell and his colleagues have revised their protocols to minimise this risk.
They are also working on speeding up the process. At present, it takes several weeks for the harvested cells to be re-engineered, but the team believes it could cut down processing time to nine days or less. This would also boost the cells’ potency, and could involve the addition of a kill switch that would deactivate them in the event of side effects. The team is planning on beginning clinical trials within the next two years.
"It allows us to generate a T-cell product that could be used for patient treatment in a very short time, perhaps only a few days," said Dr Lingfeng Liu, Fred Hutch immunotherapy researcher and lead author of the study, in a release. "That will save a lot of time for the patient because for the patient, time is very important. Sometimes tumour cells grow much faster than we can imagine."
Alternative avenues
Fred Hutch is far from the only research centre breaking new ground in this field. Professor Bonini’s team, who also reported at AAAS, studied ten cancer patients who had received bone marrow transplants and been infused with T-cells that could be tracked. They found that small numbers of the cells were still circulating 14 years later, suggesting that genetically modified T-cells could provide a long-lasting immune response.
Another, somewhat divergent, line of research involves inhibiting certain proteins that are formative in the development of tumours, therefore enabling the body’s own T-cells to proliferate. At the Wistar Institute in Pennsylvania, scientists recently found a new way to inhibit the protein STAT3, stopping cancer progression in its tracks.
"Our study describes how STAT3 plays a key role in differentiation of myeloid-derived suppressor cells (MDSC) to tumour associated macrophages (TAM), which are well known to suppress T-cell functions in cancer," explains lead researcher Vinit Kumar. "We know that T-cells are the policemen of our body. In cancer, T-cells kill the cancer cells. But, during cancer progression, T-cells become defective, partly because of expansion of MDSC and TAM. So, if we are able to find the molecule responsible, we could develop a therapeutic strategy."
It’s important to remember this work is still new. Riddell’s results, which are currently undergoing peer review, have not yet been published, and researchers have been loath to suggest a timeframe for clinical applicability.
However, given the astonishing nature of the findings, and the snowballing interest in this field, it is likely that we will be hearing a lot more about T-cells in the years to come. Over time, it is likely there will be applications not just for blood cancers but for other cancers, too.
As Riddell explained at the conference: "Much like chemotherapy and radiotherapy, it’s not going to be a save-all… [But] I think immunotherapy has finally made it to a pillar of cancer therapy."
Given the complexity of cancer research, it pays to be cautious in the face of what seems like a major breakthrough. However, in this case, it seems that the hype has a firm basis in reality.




