Approximately 422 million people have diabetes globally, which represents around 8.5% of adults in the world. It was directly responsible for 1.6 million deaths in 2016, according to the World Health Organization (WHO).
Statistics from Diabetes UK show that slightly more than 3.8 million people in the UK are currently diagnosed with diabetes. Cases have almost doubled in the past 20 years and are expected increase further to reach five million by 2025. Approximately 90% of cases are type 2 diabetes, compared to 9% with type 1, who have usually had the condition since birth.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
To tackle stigma around this largely misunderstood condition and raise necessary funds, Diabetes UK organises Diabetes Week annually in June. The WHO views diagnosis and treatment as crucial to reducing the burden of disease.
Considering immunotherapies for type 1 diabetes
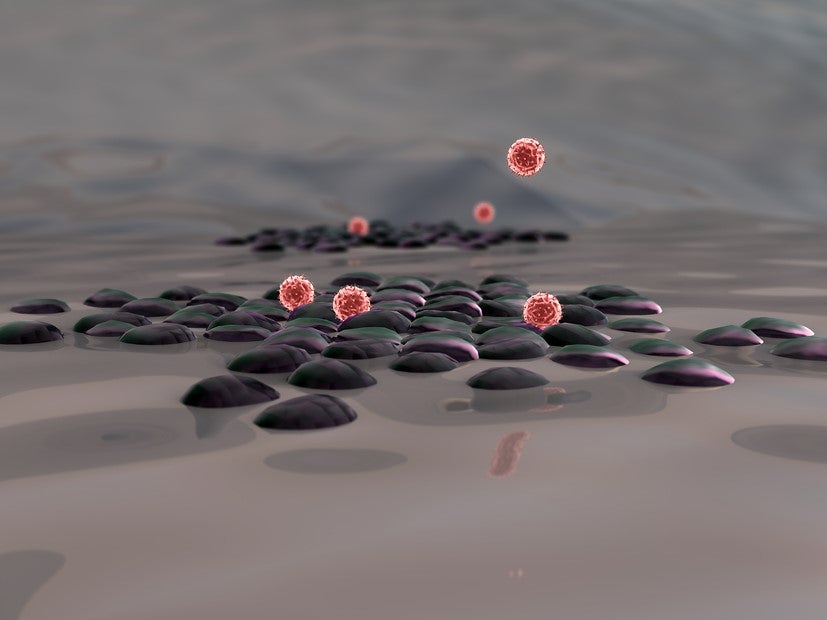
Although the cause of type 1 diabetes remains unknown, the condition leads to the immune system attacking cells in the pancreas to make insulin, therefore, when the body breaks down carbohydrates in food into glucose, this cannot be absorbed by the body.
The role of the immune system in the disease makes type 1 diabetes an autoimmune condition. However, unlike other immune system-originated conditions, such as rheumatoid arthritis and psoriasis, there has been a lack of research into therapies focusing on immune targets for type 1 diabetes. Instead treatment has focused on replacing insulin through pumps or injections.
This discrepancy spurred Diabetes UK and type 1 diabetes charity JDRF, formerly the Juvenile Diabetes Foundation, to support this therapeutic approach by setting up the Type 1 Diabetes UK Immunotherapy Consortium (T1D UK) in 2015.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataDiabetes UK director of research Dr Elizabeth Robertson stated: “Immunotherapies would represent a major shift in the way we combat type 1 diabetes – moving us from treating the symptoms to treating the cause.
“In the future, this could mean we have ways of halting the immune system’s attack in people newly diagnosed, potentially protecting them against serious complications, and of preventing the immune attack entirely in people at risk – helping to make type 1 diabetes a condition of the past.”
In the past four years the consortium has established a network of 24 research sites nationwide, which it has used alongside the UK’s research expertise to increase the number of type 1 diabetes patients taking part in research by a factor of five and to complete three clinical trials.
Renewed investment in this future treatment approach
To recognise its success to date, Diabetes UK and JDRF injected a further £490,000 into T1D UK in May this year; Cardiff University professor Colin Dayan, who leads the consortium’s research centre network, explained how money will be used.
“We will focus on making immunotherapy research bigger, smarter and faster,” Dayan said. “We plan to increase the number of clinical trials being run in the UK and make each trial more efficient, so they can be conducted in half the time and with half the number of volunteers. This will enable us to collect the evidence required to get a drug licensed, and made available in the diabetes clinic, sooner than is currently possible.”
Talking about the renewed investment, Robertson said: “Our new funding builds upon the excellent work undertaken to date by the Immunotherapy Consortium, enabling UK scientists to take bold steps and make sure the benefits of research reach people with type 1 diabetes as soon as possible.”
JDRF scientific programme manager of research Simi Ahmed added: “The Immunotherapy Consortium is positioned to become a role model in the type 1 diabetes community, increasing the amount of people who can take part in research, such that multiple trials may be run concurrently across the globe without competing with each other.
“Moreover, the model of partnership with both industry and academia uniquely positions the consortium to influence the design of future studies, allowing for an unprecedented opportunity in the field to combine and compare results from different trials.”
Repurposing immunotherapies for type 1 diabetes
The primary aim of T1D UK is to support getting type 1 diabetes immunotherapies to the market by providing a better environment for carrying out trials in the UK. The main way the consortium is fast-tracking treatments through clinical development is by repurposing immunotherapies developed for other conditions.
T1D UK is currently recruiting patient participants into the Phase II Ustekid trial of ustekinumab in adolescents within 100 days of their diagnosis; when people are first diagnosed with type 1 diabetes they still have 10-20% functioning insulin-producing cells. The aim is to help these patients produce their own insulin.
Ustekinumab was developed by Johnson & Johnson subsidiary Janssen as the branded product Stelara. It is an immunotherapy that blocks two human interleukins, IL-12 and IL-23, and is approved for Crohn’s disease, as well as adults and adolescents with plaque psoriasis and psoriatic arthritis.
According to the trial’s twitter account, 11 hospitals are currently recruiting for the trial and ten participants have been randomised since December. Funding for the study comes from the National Institute of Health Research Efficiency and Mechanism Evaluation programme.
Another of T1D UK’s clinical trials is investigating the effect of rheumatoid arthritis drug abatacept, in addition to normal diabetes medication, on the immune system of type 1 diabetes patients.
Marketed as Orencia by Bristol-Myers Squibb, abatacept is a fusion protein that prevents the activation of T cells.
Participants will have six blood tests during the trial – before, during and after treatment – to determine the immunological effect of the drug.
All patients have been now recruited into this trial by Guy’s Hospital; they include male and female adult volunteers aged 45 or younger who have been diagnosed within the last 100 days.
T1D UK’s study builds on a successful 2014 trial, which was part-funded by JDRF and carried out at Joslin Diabetes Center, Boston, US. Researchers found that abatacept had immunological benefits for up to a year after patients stopped taking the drug; they had lower HbA1c levels and higher levels of C-peptide, an indicator of insulin production.




