Earlier this year, Ecole polytechnique fédérale de Lausanne (EPFL) researchers were studying melanoma cancer cells when they made a surprising discovery. Based on the quantities of exosomes present in patients’ blood, cancer cells may be able to communicate with each other over much longer distances than originally thought.
“Our discovery was purely curiosity driven, as we had studied exosomes produced by cultured melanoma cancer cells,” says Professor Hubert Girault, who heads up the Laboratory of Physical and Analytical Electrochemistry at EPFL Valais Wallis. “The surprise was the amount of melanoma markers in the blood, considering that melanoma tumours are in the dermis and not directly in contact with the blood.”

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
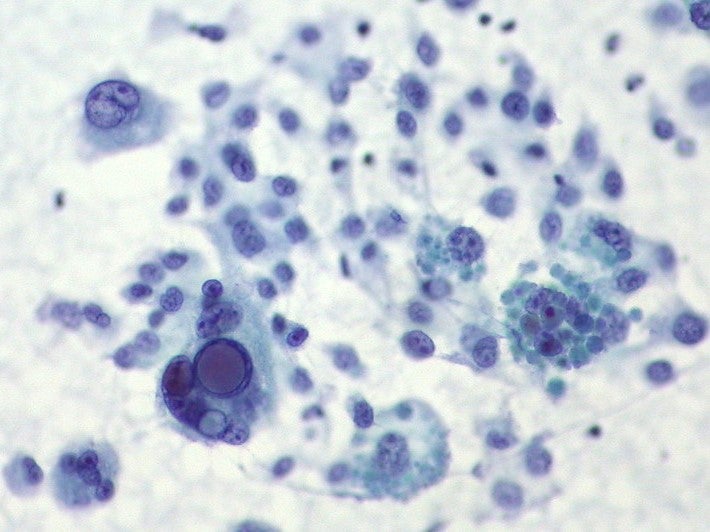
Yingdi Zhu, an EPFL doctoral assistant, had been using cell culture and mass spectrometry to isolate melanoma cancer cell exosomes. Tiny particles, around 50-100 nanometers across, exosomes are naturally released from the cell, along with a cargo of proteins, mRNA and other molecular constituents.
Although released by healthy cells too, they are emitted by cancer cells in much larger quantities, and are thought to facilitate cell-to-cell communication within a tumour.
The researchers were able to detect cancer cell markers in exosomes for each stage of melanoma growth. Using a technique known as MALDI-TOF mass spectrometry (Matrix Assisted Laser Desorption Ionisation- Time of Fight), they generated ‘exosomal fingerprints’ – a snapshot of the releasing cells and their metabolic status, which can serve as biomarkers for disease.
Next they used a kit called ExoQuick to extract exosomes from the blood. They were startled to find that the markers were present in large quantities, rather than being too heavily diluted to detect.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalData“The quantity of exosomic blood we found was very large,” says Girault. “It’s difficult to imagine that a little tumour could generate so many exosomes that would be detectable in so much blood.”
What do exosomes do?
First identified in the 1980s, exosomes were dismissed for years as a mode of cellular waste disposal – the garbage trucks of a cell. It’s only over the last decade or so that they have begun to pique researchers’ interest. Research publications increased almost tenfold between 2006 and 2015.
“The concept of exosome is relatively recent – when I was a student it didn’t exist,” says Girault. “They are now a topic of interest for the research community at large because we want to know what their target is.”
While much remains unknown about exosomes, scientists do have some ideas about their functions in the body. In essence, they appear to work as cellular messengers, communicating and transmitting macromolecules between cells. They seem to play a particularly important role in the body’s immune response, and may help promote tissue regeneration and repair.
Unfortunately, they have also been implicated in the development of several diseases. In the case of cancer, exosomes seem to play a key role in the interactions between tumours cells and the immune system, and may help tumours evade detection. As a result, they have become a hot topic among immunotherapy researchers.
“At the moment, there are many hypotheses about their role in cancer, but there is strong literature being developed about the role of the exosome in cancer cell recognition, and cell-to-cell communication,” says Girault. “In our work, we found that they survive over long distances and are stable enough to circulate in the body.”
From biopsy to blood test
The EPFL researchers’ work, published in the journal Chem, has a few important implications. First, exosomes may play a part in cancer metastasis, by sending messages through the bloodstream and preparing tissue for the spread of cancer cells.
“Melanoma has three stages, and in the third stage it becomes metastatic,” says Girault. “When we take exosomes from a metastatic tumour cell and then put them together with a cell from early-stage melanoma, we can induce the stage 1 cells to produce metastatic proteins, which shows that the exosome is involved in propagating the tumour.”
The exosomes also provide an indication of how developed a tumour is. This suggests that cancer progression might one day be diagnosed by a simple blood test as opposed to a surgical biopsy.
“At the moment, you do a surgical biopsy and analyse a slice of tissue,” says Girault. “The key question is, by doing a blood test can you have information about the presence of a tumour? At the moment it’s too early to conclude but we could say it’s a route to investigate.”
So-called ‘liquid biopsies’, he adds, could hold promise not just in cancer, but also in autoimmune diseases, cardiovascular disease and various other conditions.
“There are papers showing exosomes of many diseases are in the blood, so at the moment the hot topic is can we define strong protocols to make reliable and stable liquid biopsies? Can we identify possible tumours just by a blood test?” he says.
Liquid biopsies could hold many benefits for patients, not least tolerability and convenience. They may be able to detect disease progression long before symptoms emerge, and might even be able to predict therapeutic responses. This could revolutionise the field of cancer diagnostics and pave the way for better targeted treatments.
However, we shouldn’t get too excited just yet. As Girault points out, there are a few problems to iron out before cancer blood tests become a reality.
“It may take a while before we have a test that can be considered reliable,” he says. “One of the problems with these types of liquid biopsy is the risk of false positives. We have to ask whether the protein marker is unique to one cancer, or whether it might come from a different origin, because many cells produce similar proteins.”
Although liquid biopsies remain a matter of speculation, the EPFL team’s work represents a leap forward in our understanding of exosomes and cellular messaging.
“I didn’t think it would be possible to use exosomes to detect melanoma incidence so accurately. This breakthrough opens up new possibilities for the use of the cancer immunotherapy technique that I’m currently developing with Professor Girault,” commented Dr Ping-Chih Ho of the University of Lausanne.




