When we consider the huge problem of antimicrobial resistance, we tend to focus on bacteria and their ability to garner armour against the drugs we use to treat infection. But there’s a danger of forgetting about another significant problem in the microbial space and the very real threat it can present to hospitalised patients.
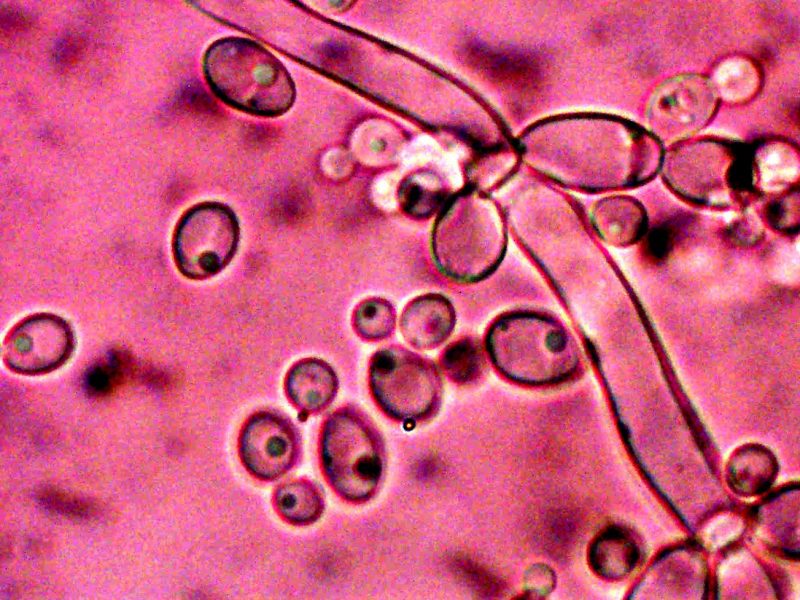
Fungal disease causes 1.5 million deaths every year worldwide. Candidiasis is one such infection, caused by the yeast Candida which normally lives on the skin and inside the body without causing any problems. If an infection develops in the mouth or vagina, we know it as ‘thrush’, which is usually mild and easy to treat.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
But for those with compromised immune systems, Candida can enter the bloodstream or internal organs, which is when the situation gets really serious. Candida auris in particular presents an emerging global threat, as it spreads easily in healthcare facilities and is resistant to many antifungal drugs.
Cidara Therapeutics CEO Dr Jeffrey Stein points out that there are several reasons fungal disease is a somewhat forgotten space compared to antibacterials.
“Fungal infections aren’t things you generally get outside the hospital,” he says. “These are things you get once you’re hospitalised for something else. Anything that can debilitate your immune system makes you very vulnerable to fungal infections.”
Stein explains that we tend to focus on the problem the patient was hospitalised for in the first place, which makes sense. But there is a tremendous unmet need for antifungal drugs for these groups of people, as some types of Candida are growing resistant to the most-used treatments.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalData“The flip side of that is there are very few antifungal drugs being developed,” reveals Stein.
This means there are few alternatives for healthcare providers if one treatment isn’t working.
Too close for comfort
The most recently approved antifungal agent was isavuconazole, marketed as Cresemba (Pfizer in Europe; Astellas in the US), which was granted FDA approval in March 2015 and EMA approval in October of the same year. The drug belongs to the azole class of antifungals and is used to treat invasive mould infections aspergillosis and mucormycosis. But Cresemba has many unwanted side effects and can cause interactions with other medications. These adverse effects are as big a problem as tackling resistance.
So why is it so hard to develop safe new drugs for fungal infections? The reason lies in the structure of fungi, Stein explains. As eukaryotes, fungi are much more closely related to human cells than bacteria, meaning anything designed to kill them is likely to be toxic to us. For instance, one of the oldest types of antifungal drugs is the polyene class, of which amphotericin is the best known. It targets fungal cholesterol. Unfortunately, fungal cholesterol is relatively similar to human cholesterol meaning the drug can cause some unwanted side effects, such as fever, low blood pressure and vomiting.
Another class is the azoles, such as fluconazole. This type of drug targets fungal cytochrome p450 enzymes involved in metabolism.
“These are the liver enzymes that are used to metabolise toxins as well as other drugs,” explains Stein. “Because patients who get antifungal drugs are usually hospitalised with something else, they tend to be on a lot of drugs. Drugs in the azole class interfere with the metabolism of these other drugs and cause drug-drug interactions. It’s a big problem.”
A new class of antifungal does hold promise though. Echinocandins target a fungal enzyme for which there is no homologue in humans. Medications in this category target a molecule that is needed for fungi to make their cell walls.
Enter echinocandin
Cidara’s candidate rezafungin belongs to the echinocandin family. It was discovered by a small company in North Carolina looking for a new antifungal that could be taken as a tablet, but they weren’t successful in developing an oral form of the drug.
Cidara was looking to acquire a compound that was ready to be put straight into clinical studies when they came across rezafungin.
“We noted three important things,” says Stein. “One: it had remarkable pharmacokinetics. The animal data suggested it could be dosed once a week. That got our attention because it would actually give it advantages over an oral drug.”
He explains that patients taking tablets tend to prematurely discontinue their treatment plan. But if you could discharge someone knowing they have a safe and effective exposure of an antifungal agent for a week, it could give clinicians greater peace of mind.
“The other thing we noticed is the remarkable efficacy. It was far more effective in animal models than other echinocandins. What we ultimately found out is that because it can be safely dosed once a week, you could provide very high exposures in patients,” he said.
Thirdly, he reveals, the drug appeared to be safer than other echinocandins, which break down in the bloodstream and cause metabolites that are toxic to the liver.
Phase I and II trials with rezafungin have shown promise, and the drug is now in two Phase III studies. One is for the treatment of candidemia (the presence of a Candida species in the bloodstream) and invasive candidiasis. The other is to see if rezafungin can be an effective preventative against fungal infections in patients who have undergone a bone marrow transplant.
“If you are unlucky enough to need a bone marrow transplant, you’re going to need antifungal prophylaxis,” says Stein.
The problem is the current regimen is a cocktail of drugs have a lot of drug-drug interactions and toxicity issues for the patient. Because of these tolerability issues, there’s a high rate of discontinuation.
“So about a third of the patients who are discharged prematurely discontinue their prescriptions. And of those that do discontinue, should they get a fungal infection, the mortality rate is 50 to 60%. That’s a coin flip of whether or not you’re going to die if you discontinue that drug regime,” Stein notes.
In September 2019, Cidara signed a collaboration agreement with Mundipharma licensing the rights to rezafungin outside of the US and Japan. The total transaction value could exceed $568m.
But if rezafungin does reach market, will resistance issues eventually become a problem for this drug too? Stein admits it’s possible. Any drug that gets prescribed a lot is going to generate resistance eventually, but Cidara has a plan to tackle this.
“Luckily we know how to engineer resistance against rezafungin as there are certain point mutations in the target that we can engineer,” reveals Stein. “And the good news is, unlike antibacterials, antifungals aren’t as prevalently used out in the populace. So you simply don’t see the same magnitude of exposures that are generally needed to evolve resistance.”




