Multiple myeloma is a difficult cancer to treat. A form of blood cancer, it is considered incurable, but the available treatments can greatly prolong the patient’s life. Almost without exception, patients receive combination therapies, consisting of several different drugs.
Often, this drug combination will include bortezomib (marketed as Velcade), a proteasome inhibitor that has greatly improved the median survival rate. Unfortunately, a number of patients are resistant to Velcade, and most others become resistant over time. This seriously restricts its efficacy.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
It can be challenging, then, to find the right drug combination for the right patient – not least because there are dozens of potential drugs on offer.
“Different patients will undergo random genomic alterations that ultimately lead to their cancer, so there’s a lot of heterogeneity,” says Dr Edward Kai-Hua Chow, principal investigator at the Cancer Science Institute of Singapore, National University of Singapore (NUS). “Pair that with the fact people are very different – different ethnicities, ages, diets – and it makes sense that all these patients respond very differently to different drug combinations.”
He adds that, when researchers look to design a new drug combination, they will test it out on a cohort of patients and hopefully find a high proportion responding favourably. However, this strategy is far from infallible.
“If you look at all the clinical trials for drug combinations in multiple myeloma, or for that matter most cancers, you’ll never see 100% response to any drug combination,” he says. “These patients are very different from each other genomically, and there’s a whole host of unexplained factors relating to lifestyle or the human body that we don’t know yet.”

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataPersonalised vs precision medicine
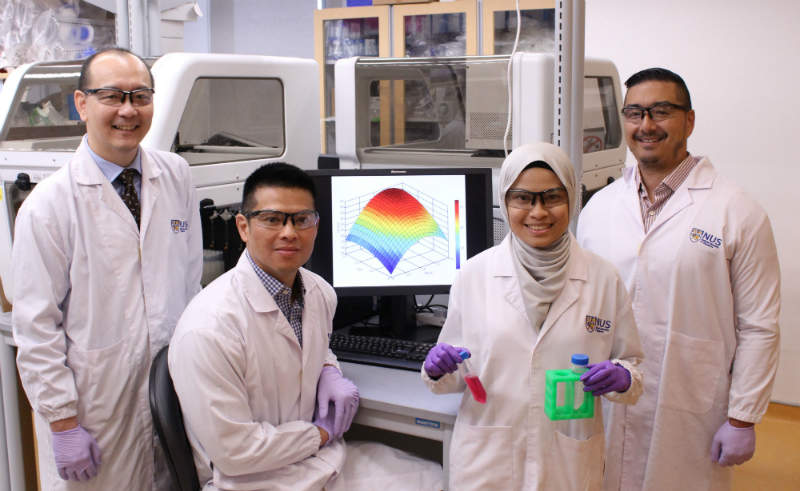
Along with colleagues at NUS, Chow recently developed an artificial intelligence platform that could change the way drug combinations are designed. The Quadratic Phenotypic Optimisation Platform – otherwise known as QPOP – is intended to speed up drug combination design and home in on the best combination for each patient.
By taking a small sample of blood or bone marrow, the platform is able to map how certain combinations of drugs will affect each person’s cancer cells.
“The idea is that you can mathematically derive what the best combinations are without any knowledge of exactly how the cancer works,” says Chow. “You can use a very small number of experiments to quickly identify the best drug combination to achieve your desired output – killing cancer cells or making people with cancer live longer. So it’s a very efficient small dataset analytic platform for drug combination design.”
He points out that this is different from precision medicine, in which certain genomic biomarkers are used to target drugs at patient subgroups. That strategy relies on knowing how the drug interacts with the cancer cells. The QPOP strategy, by contrast, leaves room for all the unknowns.
“It takes the idea that any biological model is a complex system, and you don’t know everything there is to know about what goes on inside the cancer cell,” says Chow. “The QPOP platform is focused on personalised medicine, where you’re saying that regardless of the genomic background of this patient, this is the best drug combination for them. It’s determined experientially through actual testing of the patient’s sample.”
Improving the standard of care
Chow’s team, who published their findings in the journal Science Translational Medicine in August, started with a pool of 114 FDA-approved drugs. From these, the QPOP platform was able to identify several effective drug combinations, which could be applied to Velcade-resistant cancer cell lines.
One of these combinations was completely new and unexpected, and (as demonstrated on 13 patient samples) outperformed the standard of care regimen for Velcade-resistant multiple myeloma. The platform was also used to discover the optimal dosage ratios of the drugs.
“Velcade is the backbone of all drug combinations in multiple myeloma, and if you can overcome resistance to that that then you can improve multiple myeloma therapy,” says Chow. “We showed that using the QPOP can efficiently identify a novel drug combination that helps improve the standard of care regimen.”
The researchers then took four additional patient samples, and used the QPOP platform to identify the optimal drug combination for each sample.
“What you get is a ranked list of the absolute best combinations and worst combinations as well as an understanding of all the interactions of all the drugs in the list,” says Chow. “From that we’re able to rank the potential drug combinations for different patient samples, and identify what would potentially be the best drug combination for that patient.”
The journey to the clinic
Ultimately, QPOP could have two potential applications. The first lies within drug development – especially as more targeted drugs hit the market, many of them require a companion drug or drugs. QPOP could be used to quickly and cost-effectively identify the best combination therapies to use with a novel targeted agent.
The second, and more long-term, goal is to better tailor treatments for individual patients.
“We would run the QPOP platform on the patient sample, and from that information QPOP would be able to suggest potential combination therapies that the patient should be more sensitive to,” says Chow.
The researchers are already beginning to look at translating their research to the clinic. They intend to recruit patients for prospective clinical trials, as well as expanding the platform’s application into disease areas beyond multiple myeloma.
“We’re looking to find out the feasibility of applying QPOP towards patient samples, and then we’re hoping to start clinical trials within the next couple years,” says Chow. “We will try to investigate whether having QPOP guide drug combination choice really benefits the patients’ outcome.”
He adds that conventional cancer therapies tend to treat patients as the same – they receive the same combinations of drugs in the hope that these will work. Clinicians are forced to adopt a trial and error approach, with varying success.
“There’s no real platform right now that actually takes the patient’s own cancer cells and specifically uses that to design the best combination for that patient,” he says. “But ultimately we want to move towards truly personalised medicine.”




