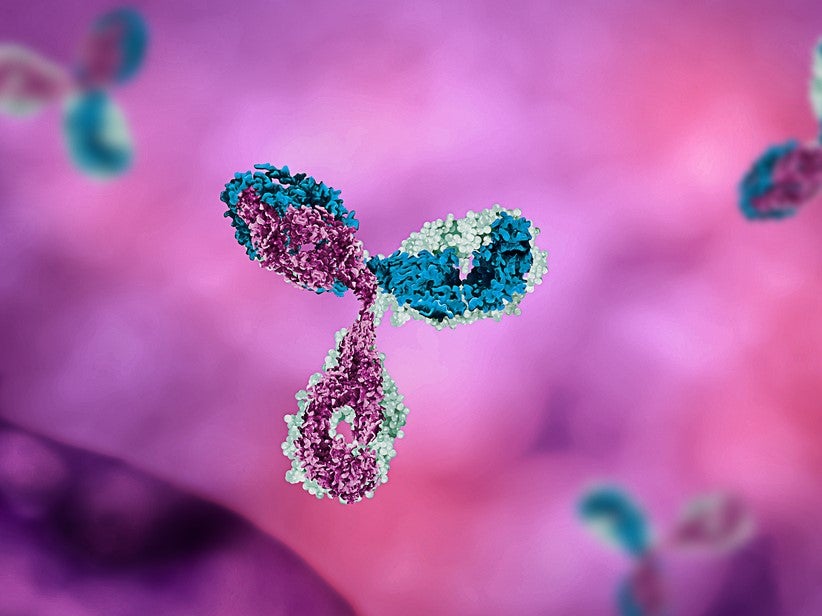
Antibody-drug conjugates (ADCs) hold the potential to change the nature of cancer treatment. Unlike classic chemotherapy – in which a drug is released into the body, killing cancer cells and healthy cells alike – ADCs enable the drug to be transported selectively to the site of action.
In essence, a cytotoxic drug is linked to an antibody, which homes in on a given protein (antigen) found only on tumour cells. Once the antibody has found its target, the tumour cell absorbs the molecule, which releases its toxic payload in the right place. At least in principle, this means killing the cancer while sparing healthy tissue, limiting side effects.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
“In addition to being a classical therapeutic antibody, the antibody within ADCs needs to trigger internalisation into the cell upon target binding and maintain a high level of stability,” explains Marc-André Kasper, a researcher at the Leibniz-ForschungsInstitut für Molekulare Pharmakologie (FMP) in Berlin. “Meanwhile, the small molecule payload needs to be highly potent due to low concentrations of ADCs in cells.”
In recent years, there has been much discussion around ADCs, and there are more than 200 drugs of this kind at the clinical or preclinical stage. So far, six have been approved, including four in the past two years, and there are several others at the late stages of development.
One particularly exciting candidate is a molecule called DS-8201, which is being developed by AstraZeneca and Daiichi Sankyo. This drug is expected to become one of the biggest cancer biologics and could replace the breast cancer drug Herceptin.
While the concept is certainly promising, these drugs are often tricky to manufacture. As Kasper explains, ADCs combine the complexity of two worlds: small molecule chemistry and antibody biology. Then there’s a third factor, the linker that connects the two. This needs to be stable during circulation in the blood and yet capable of unloading the drug in tumour tissue.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalData“To be effective as a therapeutic for any indication, the ADC must be designed considering the appropriate combination of antibody, linker and payload,” he says. “It needs to take into account their individual and combined properties. Only then can we succeed in developing ADCs with a broad therapeutic window that generates added value for the patient.”
The missing link
Up to now, the biggest issue with ADCs has been that they lose a high proportion of their toxic cargo in the bloodstream, rather than waiting to deposit it in the cancer cell. The culprit here is a faulty linker.
“The linker design has been a challenge in ADC development,” says Kasper. “Premature cleavage of the payload into the blood due to an unstable linker can cause severe side-effects and limits the therapeutic window of current ADCs.”
This is why the first generation of ADCs was unsuccessful in avoiding side effects. While the first ADC, Mylotarg, was approved as early as 2001, it was later withdrawn – the drug was being unloaded into patients’ bloodstreams at a sometimes fatally toxic dose. It was reapproved in 2017 at a lower recommended dosage.
Kasper, along with colleagues at the FMP and the Ludwig-Maximilians-Universität München (LMU), is working on solutions to this problem. In two recent papers published in Angewandte Chemie, his team discussed a new linker technology that could better stabilise the link between drug and antibody.
“We believe that linkage stability is one of the crucial aspects for developing the next generation of ADCs,” says Kasper. “In addition to that, previous research has shown that nonpolar linker-drug combinations limit the number of drug molecules that can be added to the antibody. So we aimed to increase the polarity of our linker system.”
Their technology is based on unsaturated phosphorus compounds (phosphonamidates), which can connect a given small molecule drug with the amino acid cysteine. Cysteine is naturally present in antibodies, albeit in small quantities. This means you can maintain a tight control over how the drug and antibody fuse together, and create a bond that is highly stable during systemic circulation.
“Cysteine modification is particularly interesting for the synthesis of ADCs, which has been previously demonstrated and applied to two of the approved ADCs on the market,” says Kasper. “Our technology allows the construction of ADCs with an acceptable homogeneity, starting from a native antibody, without any need for elaborative engineering. We have also developed a simple way to chemically install our compounds into very complex molecules in a chemoselective way. This is a process that hasn’t been described in the literature before.”
Strong and stable
In order to test their method against others on the market, the researchers compared their technology with the approved ADC, Adcetris. Adcetris is a lymphoma drug, approved in 2017, which links the antibody brentuximab to the anticancer agent vedotin.
The team recreated this drug as precisely as possible, but replaced the drug’s existing maleimide linker with their own phosphonamidate linker. Then they applied the drug to blood serum to test its stability.
“We were able to demonstrate a drastic increase in stability with our technology,” says Kasper. “For Adcetris, we observed a payload loss of more than 75% after three days. In contrast, our linker lost less than 10% of the payload after seven days.”
From these results, the team hypothesised that a reduced dose of the redesigned ADC would be sufficient to treat mice with non-Hodgkin lymphoma.
“We were pleased to observe an increase in the median survival of the mice group treated with our redesigned phosphonamidate-linked Adcetris construct by more than two-fold compared to the group treated with Adcetris,” says Kasper.
The road to commercialisation
Evidently, this technology could go a long way towards improving the safety and stability of ADCs.
“We have a lot of evidence that our method can solve some of the limitations that are currently associated with ADC treatment,” says Kasper. “It allows us to significantly reduce premature cleavage of the payload and reduce ADC dosing while still achieving a sufficient anti-tumor effect in mice. This means it has the potential to reduce side-effects and widen the therapeutic window of ADCs.”
Having demonstrated the technology in vivo, the researchers are now performing additional stability studies to improve their understanding of how it works.
“In addition, we are further optimising our linker system chemically. The rather unusual phosphorus-based structure still gives us a lot of room to play with and to implement new linker properties that are inconceivable with commonly applied linker systems,” says Kasper.
They have also founded a spin-out company, Tubulis, which will take the technology further, driving it towards market maturity.
“Tubulis is commercialising the technology and applying it to identify novel, uniquely matched antibody-drug combinations,” says Kasper. “Its chemical flexibility enables us to quickly identify perfectly matched ADCs that overcome current limitations in the field and deliver a better outcome for the patient.”




