Systemic lupus erythematosus (SLE), a devastating auto-immune disorder that predominantly affects young women of child-bearing age, can be a fatal disease if left untreated. Because there is currently no cure for SLE, patients suffering from this disease will most likely take multiple immune-suppressing medications over the course of their lives.
The life expectancy for those living with SLE has almost doubled during the past 50 years, with survival rates now approaching 90%. Improved supportive treatments, particularly the increased use of antimalarial therapy, are among the main drivers for this prolonged survival.
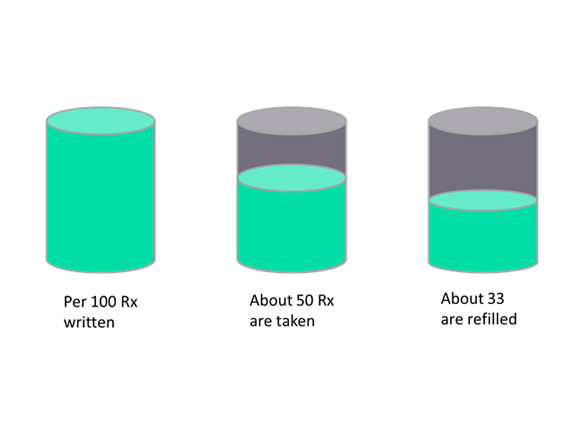
Worryingly, a recent systemic review of the literature identified 11 studies covering self-reported surveys, electronic monitoring devices, clinical records, and prescription refill sources that showed that more than half of all lupus patients are not taking their medication. Antimalarial therapy showed particularly low compliance rates.
Although this finding seems initially surprising, because antimalarials are known for their long-term beneficial effects and good safety profile, GlobalData notes that their therapeutic onset is slow and their benefits are not associated with the reduction of primary symptoms experienced by patients. While a review of the literature identified depression, rural residence, lower education levels, and polypharmacy as major determinants of low compliance, physicians and expert interviewed by GlobalData were particularly concerned about young people simply not wanting to take their medication.

Low compliance to prescribed medication is a tremendous problem for the long-term survival of lupus patients, and while the studies only identified patient-centric causes for poor compliance, GlobalData believes that the treatments themselves are equally to blame. Treatment options for lupus are sup-optimal, with high daily pill burdens and an increased rate of treatment-associated side effects over time, particularly for steroids. New, improved treatment options for lupus are therefore eagerly awaited by both physicians and patients alike.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataGlobalData identified six promising pipeline drugs in clinical development for lupus, most of which benefit from a weekly, biweekly, or monthly dosing schedule, therefore reducing the overall pill burden by replacing daily regimens. All of these investigational drugs have the potential to transform the lupus treatment landscape in unique ways over the next decade.