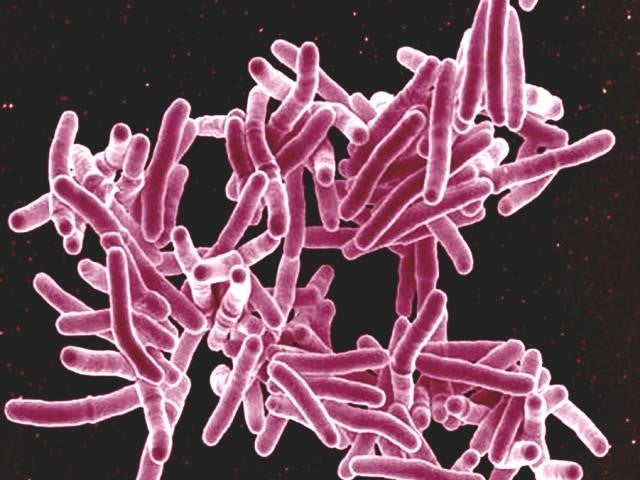
Drug-resistant tuberculosis (DR-TB) is a serious, and growing, public health threat. Despite attracting less media attention than other diseases of comparable severity, TB is the world’s deadliest infectious disease and the drug-resistant strain is becoming more virulent.
Worldwide the disease infected 558,000 people in 2017, and killed 230,000. By 2050, the mortality rate could soar to 2.5 million – a more than tenfold increase. This would cost the global economy $17tn.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
“DR-TB is an epidemic within an epidemic,” says Cat Oyler, vice president of global public health, tuberculosis, at Johnson & Johnson. “If we don’t address DR-TB now, research has shown the proportion of DR-TB will continue to increase, becoming more and more difficult and more and more expensive to treat.
In May, The Economist Intelligence Unit (EIU) released a report on the subject, sponsored by Johnson & Johnson. The report – subtitled ‘the case for action’ – did not sugarcoat the facts. It pointed out that our current response to the situation is far from adequate, and made a strong case for increasing investment into DR-TB.
“We need to start treating this disease like the public health emergency that it is. And this means that we urgently need to challenge the status quo,” says Oyler. “All sectors – public, private, not-for-profit and, importantly, affected communities – need to come together to solve this problem in new and innovative ways.”
The burden of DR-TB
When we think of tuberculosis, we may be tempted to dismiss it as a Victorian disease. Until the mid 20th century, TB was a well-acknowledged public health problem with no medicinal cure. It was known variously as ‘consumption’, ‘phthisis’ and ‘the White Plague’, and was especially prevalent among the urban poor.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataFollowing the arrival of the first TB drugs, both incidence and mortality rates plummeted, raising hopes that the disease could be wiped out altogether. Unfortunately, by the 1980s the first drug-resistant strains had emerged.
“DR-TB are strains of the disease that are resistant to the most commonly used TB treatments – including, but not limited to, rifampicin and isoniazid,” says Oyler. “Today, DR-TB is the largest contributor to antimicrobial resistance (AMR), accounting for one-third of all AMR-related deaths.”
Today, TB itself kills 1.6 million people every year, more than HIV and malaria combined. Perhaps unsurprisingly, the vast majority of these deaths (more than 95%) occur in developing countries, which are under-resourced. In 2018, there was an estimated $3.5bn shortfall in the $10bn budget required to address the disease.
“Because the disease is airborne, people who are in close contact with people who have been recently infected and those with a weakened immune system are at a higher risk of contracting TB,” says Oyler.
In the past, the drug-resistant strains developed when people didn’t complete their course of medicine. However, we are now seeing more person-to-person transmission of DR-TB, which Oyler describes as ‘a concerning trend’.
“One of the main issues is that only one in three people with DR-TB are diagnosed and one in four people are treated. In effect, this means that there are approximately 400,000 people with DR-TB who don’t even know they have it,” she says. “To make matters worse, one untreated person can infect ten to 15 others over the course of a year through close person-to-person contact, making this a major global health security threat.”
Mobilising resources
Given all the discussion around antimicrobial resistance, it is nothing short of bizarre that DR-TB has been so underlooked. The EIU report makes it clear that, if we want to successfully combat AMR, we have to start with DR-TB.
“We need to focus on reaching more patients with the tools we have today – by diagnosing them and connecting them with care as early as possible,” says Oyler. “And we need to develop even better tools for tomorrow’s patients, including rapid, point-of-care diagnostics; shorter, more effective and better tolerated treatment regimens; and eventually a preventive vaccine.”
This is more than just a pipe dream. We only need think back to the Ebola crisis to see what might be possible – when the global community comes together to mobilise resources, we consistently see results very fast.
What’s more, we do already have treatments that are effective against DR-TB. In 2012, Johnson & Johnson launched bedaquiline, the first new TB medicine in over 40 years. One of the last lines of defence against TB, it works by blocking an enzyme in the TB bacterium, meaning it can no longer generate energy. It is always used in combination with other TB drugs.
To date, J&J has delivered more than 100,000 courses of bedaquiline across 120 countries. It has also worked closely with governments and partners in high-burden countries to strengthen TB healthcare delivery systems. This has meant training health workers, improving diagnostic capacity, and raising awareness about TB at the community level.
“Making our medicine available and accessible to patients in need in a responsible way is – and always has been – our top priority,” says Oyler. “In 2015, in an effort to help developing countries build the capacity needed to introduce a new TB medicine, J&J launched a four-year bedaquiline donation programme for up to 110 eligible countries.”
The time to act is now
The company has also announced a ten-year initiative, in support of the global target of ending the TB pandemic by 2030. The goal is to save an estimated 1.8 million lives and prevent 12 million new TB infections in the next decade.
“Johnson & Johnson is committed to stay in the fight against TB for the long haul,” says Oyler. “We are working with partners across the globe to improve detection of undiagnosed cases of TB, broaden access to our novel medicine for multidrug-resistant TB, and accelerate research & development to discover next-generation TB treatments. Experts agree that we can’t end the TB pandemic with today’s tools alone, and that more innovation is urgently needed in this space.”
From a health economics perspective, investing in DR-TB makes a lot of sense. As the EIU report explains, the benefit-to-cost ratio has been estimated as up to $23 for every dollar invested. This factors in the costs associated with mortality, absence from work, and threats to tourism and public infrastructure.
In short, the cost of inaction is high – and as DR-TB becomes more prevalent, it’s likely to get higher. The EIU report makes a compelling case that the time to act is now.
“We have never been better placed to end TB – we have better tools, game-changing science and greater levels of political commitment than ever before,” says Oyler. “Together, we can stop the world’s biggest contributor to antimicrobial resistance and drive progress toward a world without TB.”




