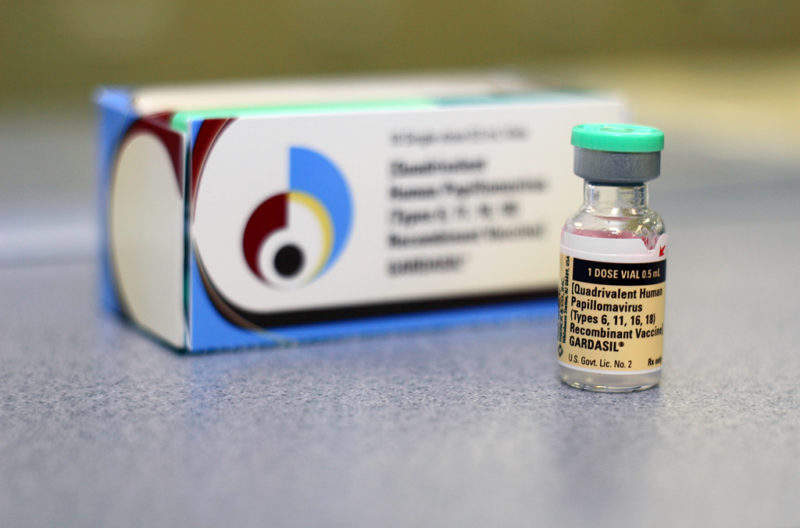
Early in October, the FDA approved Gardasil 9 (Human Papillomavirus [HPV] 9-valent Vaccine, Recombinant) for expanded use to include men and women ages 27 through 45 years.
This approval provides a great opportunity for the US to decrease or potentially eliminate HPV-related cancers, as Australia is already on the path to do. The expansion of Gardasil to older age groups provides a new way for the US to combat HPV-related cancers, especially since the US is still far behind other countries in vaccination completion rates for adolescents.
HPV infection is very common; most people who become sexually active will have been infected by a string of HPV within two or three years. The HPV vaccine was originally recommended for adolescents because the vaccine has a better immune response in the younger age groups and is more effective before exposure to any HPV infection.
A study by Gertig and colleagues published in the British Medical Journal found that vaccination before 14 years of age reduced high-grade cervical dysplasia five years after vaccination by 75%. The reduction in high-grade cervical dysplasia was only 32% in those who were vaccinated at 17 years of age. For those vaccinated later in life, efficacy is expected to be even lower.
However, a study with a broader definition of efficacy conducted in approximately 3,200 women ages 27 through 45 found that the vaccine was also 88% effective in preventing various HPV-related diseases such as persistent infection, genital warts, vulvar and vaginal precancerous lesions, cervical precancerous lesions, and cervical cancers related to HPV types covered by the vaccine within three and a half years. The FDA’s decision to approve for older age groups was based on this study, its long-term follow-up data, and several other studies in men.
The American Academy of Pediatrics estimated that each year, without vaccination, the annual burden of genital HPV-related diseases in US women includes 1.4 million new cases of cervical intraepithelial neoplasia 1 (CIN1), 350,000 new cases of genital warts, and 330,000 new cases of CIN2/3, which is estimated to cost $7B in medical care.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalData
In addition, HPV-related throat cancers are also expected to increase in the next decade. GlobalData also estimated that oropharynx cancer is expected to increase by almost 3% per year from 2016–2026. A significant majority of the medical burden and the morbidity and mortality associated with these diseases can be avoided since 70%–90% of cervical and throat cancers are attributable to HPV.
While the US has seen significant improvements in HPV vaccination initiation in adolescents and young adults over the past decade, such as a near-quadruple increase in vaccination rates for one dose or more in men from 2011–2016, the UK and Australia have much higher completion rates. The figure below shows the coverage of three or more doses in the US, the UK, and Australia. The UK and Australia are seeing 80%–90% of the adolescent population starting and completing the HPV vaccine series, while the US is only hitting around 50%.
The expanded approval in the US may help in the fight against HPV-related cancers. However, the approval does not equate to recommendation, as the medical organizations that make such vaccine recommendations still require more data to see the vaccine’s effects in the target older adult population. Since it takes more than 10 years for HPV infections to become cancerous, we currently do not have sufficient data to analyse the direct impact of HPV vaccines on HPV-related cancers. The focus in the US may continue to remain on adolescent vaccination.