As policy-makers examine a range of options to address concerns about high drug prices in the United States, many are giving renewed attention to the differences in prices between the US and ex-US countries, and are considering deploying coverage and payment tools used in ex-US countries (e.g., cost-effectiveness analysis) to control costs. In this context, it is increasingly important to understand whether ex-US models of drug access hold implications for patient outcomes if they were applied in the US.
Our analysis indicates that, if the access models representing five ex-US comparator countries (Australia, Canada, France, South Korea, and the United Kingdom) were to replace the actual US access conditions between 2006 and 2017, aggregate survival gains (i.e., gains in life years) due to innovative medicines would have been cut in half for US patients diagnosed with locally advanced and metastatic NSCLC. This reduction in health gains is due to the access delays experienced by patients in other countries compared to patients in the US.
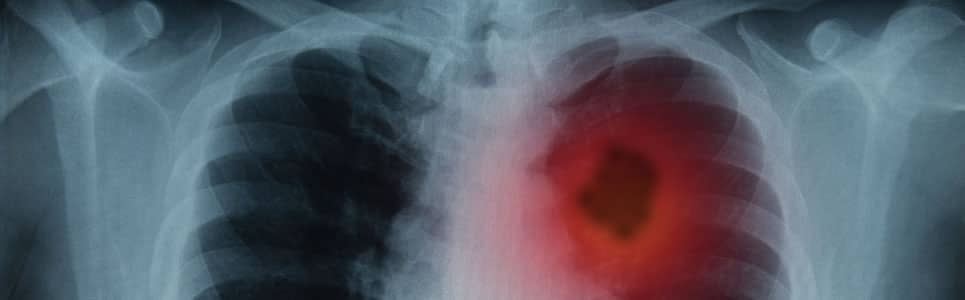
This study quantifies the population health impact in the US of introducing non-US models of drug access to an American patient population with locally advanced or metastatic non-small cell lung cancer (NSCLC) between 2006 and 2017. The model simulates the lifetime health outcomes of the target patient population under the actual US access landscape vs. five additional scenarios where US access conditions are replaced by those in the five comparator countries (i.e. characterized by the respective reimbursement approval delays and coverage gaps).
Under each alternative access scenario, the model controls for differences in regulatory approval timelines between the US and other countries. The population health impact of transposing alternative access models to the US is therefore driven by differential rates of coverage and delays in effective first date of reimbursement of the therapies in question.
Model outcomes indicate that American patients diagnosed with locally advanced and metastatic NSCLC between 2006 and 2017 have gained 201,700 life years in total due to access to innovative medicines. They would lose half of this survival benefits if they were living in the other countries.
Moreover, significant discrepancies remain between the access conditions of different countries, with the Australian system leading to the biggest drop in life years at -74% compared to the default US system.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataLastly, a large majority of the life years gained can be attributed to the non-squamous patient population. On a per capita basis the non-squamous population improved their overall survival by 73% due to innovative medicines, compared to 10% improvement in the squamous population. This speaks to the importance of continued investment in the research and development of precision medicines targeting underserved patient subgroups.