Key findings:
- In 2018, cardiovascular mortality rate attributable to cold and hot temperature among people age 65 and older tend to be highest in the southern part of the U.S. This pattern is mainly driven by the effect of heat on health.
- However, looking at the absolute count of cardiovascular mortality attributable to cold and hot temperature, the burden tends to be more spread out. Counties with higher number of residents age 65 and older tend to carry more of the mortality burden.
- Unsurprisingly, counties in the southern part of the U.S. that have greater number of residents age 65 and older (e.g. some counties in California), have the highest count of cardiovascular mortality attributable to cold and hot temperature.
- Assuming business-as-usual future scenario (RCP 8.5), we estimated increasing threats of climate change on population health in some of the most heavily impacted states (e.g. California) even within the next 10 years.
Interspersed with the COVID-19-dominated news, the many recent policy changes that weaken the clean air and climate change regulations in the United States have been hotly discussed. Along with the coronavirus pandemic, this flurry of environmental policy shifts could also have a long-lasting impact on population health.
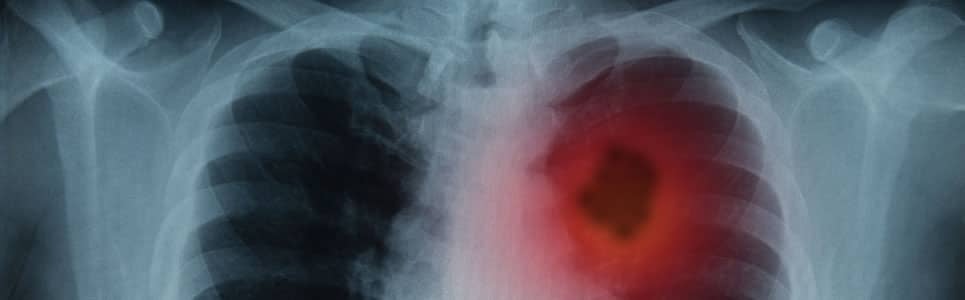
Climate change is a global health issue that has been linked to numerous adverse health outcomes, including heat-related illnesses, respiratory diseases, and cardiovascular diseases (CVD). Climate change affects health through several known pathways, one of which is through increasing human’s exposure to more extreme temperatures. Factors that increase one’s vulnerability to extreme temperature include older age, geographical location (e.g., living in heat deserts without adequate shade), pre-existing health conditions, and insufficient access to resources (e.g., inability to afford air conditioning ). In the United States, 56 million people are currently age 65 or older, with this number projected to reach 95 million—23% of the total population—by the year 2060.
Our Climate Change Health Impact Model is designed to quantify the impact of climate change on morbidity and mortality burden, as well as illustrate costs associated with these attributable health outcomes. Quantifying the health and economic consequences of climate change is key to raising public awareness and informing policy. In this analysis, we looked at the potential effect of climate change-induced fluctuations in ambient temperature on cardiovascular mortality among people age 65 and older in the United States.
The predictive model was constructed using 22.3 million mortality records from 1979-1988 National Vital Statistics System (NVSS) Mortality Data, which includes daily time and geographical details in its open access dataset. We used 1979-1988 mortality data as it provides day and county indicators in its open access dataset. Access to these indicators are restricted in more recent dataset. Using the provided geographical and time indicators, we combined this dataset with corresponding meteorological data gathered by the National Climatic Data Center (NCDC). Distributed lag non-linear models were constructed to produce county-level relationships between daily temperature and CVD-related mortality that also capture the potential delayed effect of ambient temperature. The baseline relative risk functions are set at 32°F, which allow the functions to capture both harmful and beneficial effects of hot and cold ambient temperature on CVD-related mortality risks relative to this baseline temperature.
We used the 2018 daily meteorological data to estimate the attributable CVD-related mortalities among people age 65 and older in 2018. Aggregating results from our county-level analyses, we estimated 55,000 (7.9%) CVD-related mortality among people age 65 and older in 2018 were attributable to exposure to cold and hot temperature. Putting these results into context, it is important to keep in mind that CVD mortality is only one of the many potential health outcomes that could be attributable to climate change. Thus, the total impact of climate change on population health is likely to be much greater.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalData
In addition, our findings suggest that the changing temperature due to climate change affect regions of the U.S. differently. Not only that, it also affects subgroups of people living within these regions disparately. For example, in our analyses, California was shown as one of the states that would be most affected by the impact of climate change on CVD-related mortality. In 2018, approximately 8,400 CVD-related mortalities amongst Californian resident age 65 and older are attributable to hot and cold temperature. If we are to assume future temperature follows business-as-usual scenario (RCP 8.5), the projected CVD-related mortality count jumps to 9,900 mortalities attributable to hot and cold temperature in 2030. This further highlights the increasing threats of climate change in the imminent future.
The COVID-19 pandemic has spurred calls for deregulation on climate-related issues in hopes of increasing job opportunities for America’s workforce. Waiving environmental requirements that contribute to climate change could, however, contribute to higher mortality among the nation’s older population.
This research was conducted by Cynthia Siego, Sr. Consulting Analyst, Life Sciences, IHS Markit